Pregnancy-related deaths have emerged as a pressing public health concern in the United States, with alarming trends revealing that the national maternal mortality rate is the highest among high-income countries. A staggering 80% of these deaths are preventable, highlighting the urgent need for improved prenatal care and comprehensive postpartum support. Research indicates that between 2018 and 2022, the maternal mortality rate rose significantly, revealing stark racial disparities that cannot be overlooked. Women of color, particularly American Indian and Alaska Native populations, face the highest risks, illustrating the inequities within our healthcare system. Addressing this crisis requires a multifaceted approach that ensures equitable access to pregnancy health resources, emphasizing the importance of targeted interventions to reduce preventable deaths and improve outcomes for all mothers.
The issue of maternal fatalities during pregnancy is increasingly recognized as a critical health challenge, reflecting broader systemic issues within the healthcare landscape. Terms such as maternity mortality and complications during childbirth demonstrate the complexity of this phenomenon, necessitating an in-depth exploration of its causes. From inadequate prenatal support to insufficient postpartum care, various factors contribute to these alarming statistics. Moreover, disparities in health outcomes based on race and socioeconomic status paint a daunting picture of the maternal health crisis in the U.S. Tackling these issues effectively means re-evaluating healthcare practices, policies, and accessibility to ensure every woman receives the care she deserves throughout her pregnancy journey.
Understanding the Rising Maternal Mortality Rate in the U.S.
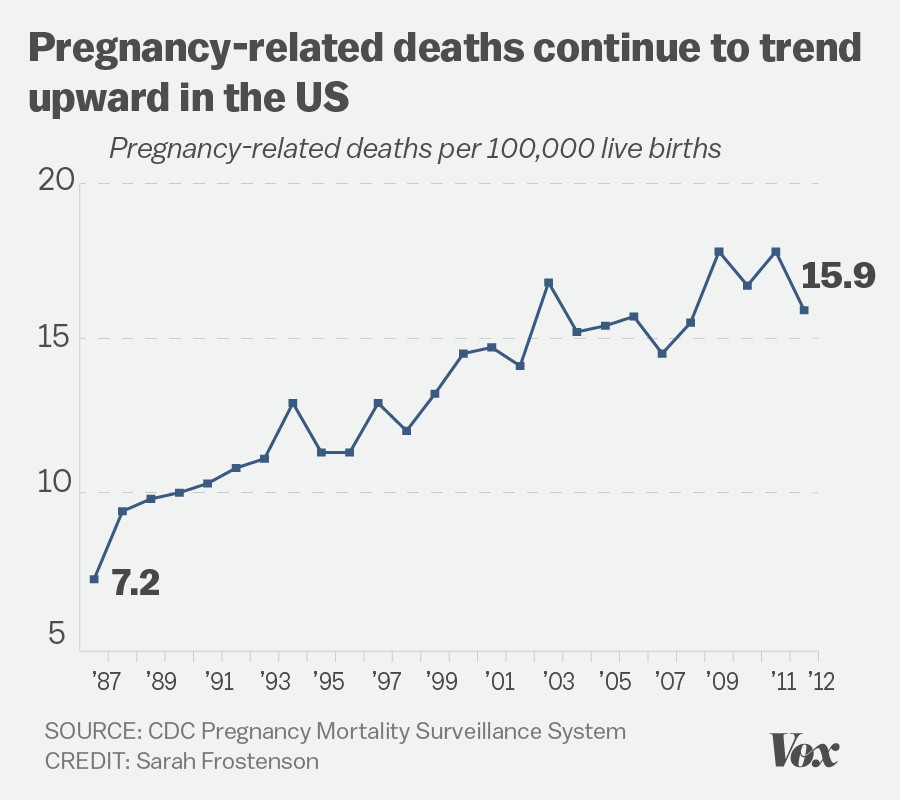
The maternal mortality rate in the United States has become a pressing concern, especially in recent years when statistics indicate a consistent rise. Approximately over 80 percent of pregnancy-related deaths are deemed preventable, placing the U.S. at the top of the list amongst high-income countries for maternal fatalities. Factors contributing to this disturbing trend include socioeconomic disparities, insufficient access to healthcare, and the lack of effective prenatal and postpartum care—elements that are essential for every pregnant individual. The U.S. healthcare framework, which can often be inconsistent and inequitable, additionally exacerbates these issues.
Research demonstrates that the most significant rise in pregnancy-related deaths coincided with the onset of the COVID-19 pandemic, highlighting the vulnerability of pregnant individuals during crises. While the mortality rate in 2022 stood at 32.6 deaths per 100,000 live births—a noted increase from 2018—it underscores the urgent need for systemic reform in how pregnancy health is managed. It’s critical that the origins of these preventable deaths be addressed through targeted healthcare reforms, increased awareness, and enhanced support systems for expectant mothers.
Race and Disparities in Pregnancy Health
Racial disparities in health are stark when it comes to pregnancy-related deaths in the U.S., with American Indian and Alaska Native women facing the highest risk. Their mortality rate is alarmingly high at 106.3 deaths per 100,000 live births, nearly four times higher than their white counterparts. This reality signals a need for focused legislative and community initiatives to improve healthcare access and equity among racial groups. Addressing these disparities requires that health professionals and policymakers work together to dismantle the systemic barriers that contribute to poorer outcomes for specific populations.
Despite the progress that some regions, like California, have made in reducing maternal mortality, the inconsistency across states highlights a troubling lack of standardization in healthcare quality. It’s evident that successful interventions can lead to improved outcomes in maternal health, yet the overall statistics reveal a concerning trend. Policies aimed specifically at reducing racial disparities and enhancing maternal healthcare could significantly contribute to reducing overall mortality rates, making it imperative that the focus on equity in health becomes a priority for lawmakers and healthcare providers alike.
The Importance of Comprehensive Postpartum Care
The postpartum period is a critical time for recovery yet often receives insufficient attention in maternal care discussions. Recent findings indicate that nearly a third of pregnancy-related deaths occurred during the late maternal period, which extends up to one year after childbirth. This timeframe is crucial for monitoring chronic conditions and ensuring that mothers receive adequate support and resources during their recovery. The current healthcare system tends to concentrate on the immediate weeks following birth, neglecting ongoing health challenges that may arise thereafter, underscoring the necessity for a continuum of care.
Adopting a broader definition of maternal mortality to include late maternal deaths could promote greater awareness and policy changes. By recognizing this extended timeline, healthcare providers can develop more effective postpartum care strategies, including mental health support, chronic disease management, and regular health screenings. Ensuring comprehensive postpartum care can help to significantly lower preventable deaths by addressing potential health issues before they escalate, ultimately contributing to better maternal health outcomes.
Innovative Solutions for Reducing Pregnancy-Related Deaths
There is a pressing need for innovative solutions to tackle the rising rates of pregnancy-related deaths. Enhanced strategies to improve prenatal care quality and extended postpartum support must be prioritized. This includes leveraging technology to enable better communication between patients and healthcare providers, as well as implementing community-based programs that provide essential resources to expectant mothers. Investment in maternal health infrastructure can lead to breakthroughs in care delivery and empower women with the knowledge needed to advocate for their health.
Public health funding must be directed towards initiatives specifically designed to reduce pregnancy-related deaths and improve maternal health outcomes. Stakeholders, including community organizations, healthcare professionals, and policymakers, should collaborate to create evidence-based policies that address the complexities of maternal mortality, particularly among marginalized populations. By refining healthcare delivery and targeting the social determinants of health, we can foster an environment conducive to safe pregnancies and healthier mothers.
Addressing the Role of Cardiovascular Disease in Maternal Mortality
In recent years, cardiovascular disease has emerged as the leading cause of pregnancy-related deaths, surpassing hemorrhage as the primary concern. Factors such as rising rates of hypertension and other chronic conditions among younger women contribute to this unsettling trend. Increased awareness of these health issues during pregnancy is paramount, as many women are unaware of the potential risks associated with latent conditions. By prioritizing cardiovascular health education in maternity care, healthcare providers can better equip expecting mothers to navigate potential complications.
Monitoring cardiovascular health should become a standard aspect of prenatal and postpartum care, ensuring women receive ongoing assessments after childbirth. This approach could significantly reduce maternal fatalities attributed to cardiovascular disease. In recent studies, interventions focusing on early identification and management of cardiac conditions have shown promise in improving postpartum outcomes, advocating for a more integrated approach to maternal health that encompasses both physical and mental well-being.
The Need for Policy Reform in Maternal Health
Reforming policies that govern maternal health is vital for addressing the rising rates of pregnancy-related deaths in the U.S. Current disparities in healthcare quality and access highlight the need for comprehensive legislative changes that focus on equitable healthcare distribution. Policymakers must advocate for initiatives that ensure all mothers receive the necessary support and healthcare services tailored to their unique needs, particularly in underserved communities. Without systematic changes to the public health infrastructure, the trend of rising maternal mortality is unlikely to reverse.
Investments in maternal health policy reform should emphasize not only immediate health care access but also long-term strategies to address social determinants of health. These reforms can drive improvements in prenatal care, postpartum monitoring, and overall maternal health education, ultimately decreasing preventable deaths. Collaborative efforts among healthcare providers, community leaders, and government agencies are essential to create a cohesive framework that will protect the health of mothers and their children throughout pregnancy and beyond.
Utilizing Data to Track and Improve Maternal Health Outcomes
The establishment of a national system for tracking maternal deaths has been a pivotal step toward understanding and addressing maternal mortality in the U.S. Since the implementation of the pregnancy checkbox on death certificates, healthcare research can now gain clearer insights into pregnancy-related fatalities, enabling more accurate reporting and analysis. Data plays a crucial role in identifying trends, disparities, and factors contributing to maternal death, ultimately guiding evidence-based initiatives aimed at improving maternal health outcomes.
In-depth data analysis can help identify specific populations at risk, allowing for targeted interventions that specifically address the unique challenges faced by vulnerable groups. By consistently monitoring maternal health statistics, healthcare organizations can adjust their practices and policies to better serve expecting mothers, yielding improved results across demographic lines. Furthermore, transparent sharing of data among stakeholders can foster collaboration and innovation in maternal health strategies, paving the way for significant advancements in care and prevention.
Encouraging Racial Equity in Maternal Health Services
Fostering racial equity in maternal health services is essential to decreasing the glaring disparities observed in maternal mortality rates across different racial and ethnic groups. Efforts to improve access to comprehensive care must encompass cultural competency training for healthcare providers to better understand and address the unique needs of diverse communities. Empowering women of color through education and advocacy can play a crucial role in challenging biases within the healthcare system, creating a more inclusive environment for all.
Policy frameworks should actively prioritize equitable health outcomes by implementing strategies that address social disparities. Investments should target improving access to quality healthcare facilities in racially diverse neighborhoods, as well as providing resources to support at-risk populations. Counteracting the historical inequities in maternal health requires a multifaceted approach involving community engagement, government support, and a commitment to creating a fair healthcare system that serves every individual equitably.
The Long-Term Impact of Maternal Deaths on Families and Communities
The implications of pregnancy-related deaths extend far beyond the immediate loss of life; they resonate deeply within families and communities. The death of a mother can reverberate through generations, affecting children’s health and economic stability, which ultimately hampers community growth and development. Recognizing this far-reaching impact underscores the urgency for systemic changes in healthcare policy and maternal health strategies that can ultimately save lives and strengthen families.
Supporting vulnerable families through grief counseling, financial assistance, and community resources can help mitigate the long-term consequences of maternal mortality. By investing in family-centered care, healthcare systems can better address the multifaceted needs of grieving families while also improving health outcomes for future pregnancies. Collective action that centers around nurturing families can foster resilience and recovery, contributing to healthier communities at large.
Frequently Asked Questions
What are the main causes of pregnancy-related deaths in the U.S.?
In the U.S., the leading causes of pregnancy-related deaths include cardiovascular disease, hemorrhage, and infection. Over 20% of these deaths are attributed to cardiovascular conditions, reflecting an alarming trend of rising chronic illnesses among pregnancy individuals.
How does the U.S. maternal mortality rate compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with significant disparities based on race and state. Between 2018 and 2022, the rate rose to 32.6 deaths per 100,000 live births, indicating a pressing need for improvements in both pre and postpartum care.
What role does racial disparity play in pregnancy-related deaths?
Racial disparities in health are a significant factor in pregnancy-related deaths, with American Indian and Alaska Native women experiencing the highest mortality rates. These disparities highlight structural inequalities within the healthcare system that continue to affect maternal health outcomes.
What impact do preventable deaths have on maternal mortality rates?
More than 80% of pregnancy-related deaths in the U.S. are preventable, underscoring the importance of better access to prenatal care and postpartum support. Targeted interventions could drastically reduce these preventable mortality rates.
Why is postpartum care critical for reducing pregnancy-related deaths?
Postpartum care is essential because a significant number of maternal deaths occur between 42 days and one year after childbirth. Continuous healthcare during this period can address ongoing health issues and improve recovery outcomes.
How can health systems reduce pregnancy-related deaths?
Health systems can reduce pregnancy-related deaths by investing in comprehensive prenatal and postpartum care, implementing standardized health policies, and addressing systemic biases that affect care outcomes for marginalized groups.
What initiatives could help reduce the maternal mortality rate in the U.S.?
To reduce the maternal mortality rate, initiatives must focus on enhancing healthcare access, increasing education around pregnancy health, implementing community support programs, and addressing the inequities that contribute to racial disparities in health.
What policies should be considered to improve maternal health outcomes?
Policies should aim to enhance public health infrastructure, mandate comprehensive postpartum care, eliminate maternity care deserts, and ensure equitable access to medical resources for all pregnant individuals, particularly in high-risk populations.
What data is available on pregnancy-related deaths in the U.S.?
Data from the Centers for Disease Control and Prevention, particularly since the implementation of pregnancy checkboxes on death certificates in 2018, provides crucial insights into pregnancy-related deaths, shedding light on the disparities and trends over time.
How has the COVID-19 pandemic affected pregnancy-related mortality rates?
The COVID-19 pandemic has exacerbated existing vulnerabilities, leading to a significant spike in pregnancy-related deaths in 2021. While rates have since moderated, they remain higher than pre-pandemic levels, emphasizing the need for ongoing vigilance and care improvements.
| Key Point | Details |
|---|---|
| Rising Death Rates | Pregnancy-related deaths in the U.S. continue to rise, with an increase from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable, highlighting the urgent need for better care. |
| Racial Disparities | American Indian and Alaska Native women experience the highest mortality rate at 106.3 deaths per 100,000 live births, significantly higher than white women. |
| Leading Causes | Cardiovascular disease is the leading cause of pregnancy-related deaths, accounting for over 20% of fatalities. |
| State Variations | Pregnancy-related death rates vary significantly by state, illustrating the disparities in maternal healthcare across the country. |
| Late Maternal Deaths | Late maternal deaths, occurring from 42 days to 1 year postpartum, account for a third of all pregnancy-related deaths. |
| Need for Policy Change | A comprehensive approach to policies addressing healthcare quality and access is necessary to reduce these deaths. |
Summary
Pregnancy-related deaths in the United States present a critical public health challenge as they have continued to rise, especially during the COVID-19 pandemic. With over 80% of these fatalities being preventable, addressing the systemic healthcare failures that contribute to these deaths is paramount. Significant racial disparities highlight the need for focused efforts on equity in maternal care. This pressing issue demands comprehensive policy changes and increased investment in postpartum care to mitigate the staggering statistics surrounding pregnancy-related mortality.