TIM-3 Therapy is at the forefront of innovative approaches to tackle Alzheimer’s disease by harnessing the power of the immune system. Recent studies have highlighted how this immune checkpoint molecule can be modified to encourage microglia—brain immune cells—to effectively clear harmful amyloid plaques, which are a hallmark of Alzheimer’s. By inhibiting TIM-3, researchers have observed significant cognitive improvement in mice models of late-onset Alzheimer’s disease, suggesting a promising avenue for Alzheimer’s disease treatment. As scientists delve deeper into the interplay between microglia and Alzheimer’s pathology, the potential for cancer treatment repurposing emerges, linking two critical health challenges: Alzheimer’s disease and oncological therapies. This groundbreaking research not only opens doors for improving cognitive functions but also reshapes our understanding of immune system roles in neurodegenerative disorders.
The exploration of TIM-3 Therapy signifies a pivotal shift in the landscape of neurodegenerative disease management, particularly in addressing the challenges posed by Alzheimer’s. This innovative treatment method targets specific immune checkpoint molecules, which regulate brain immune cell activities and their ability to combat the buildup of Alzheimer’s-related plaques. Effective communication between microglia and the brain’s immune framework is crucial for cognitive preservation, where alternative therapeutic strategies are now being analyzed for their utility in enhancing memory and overall brain function. As the research unfolds, it becomes evident that strategies deployed against cancer may hold transformative potential in improving cognitive health and addressing the complexities of both Alzheimer’s and other immune-mediated conditions. Such advancements could lead to novel interventions that not only help in cognitive improvement but also foster a deeper understanding of the immune system’s pivotal role in Alzheimer’s and related disorders.
Understanding TIM-3 Therapy for Alzheimer’s Disease
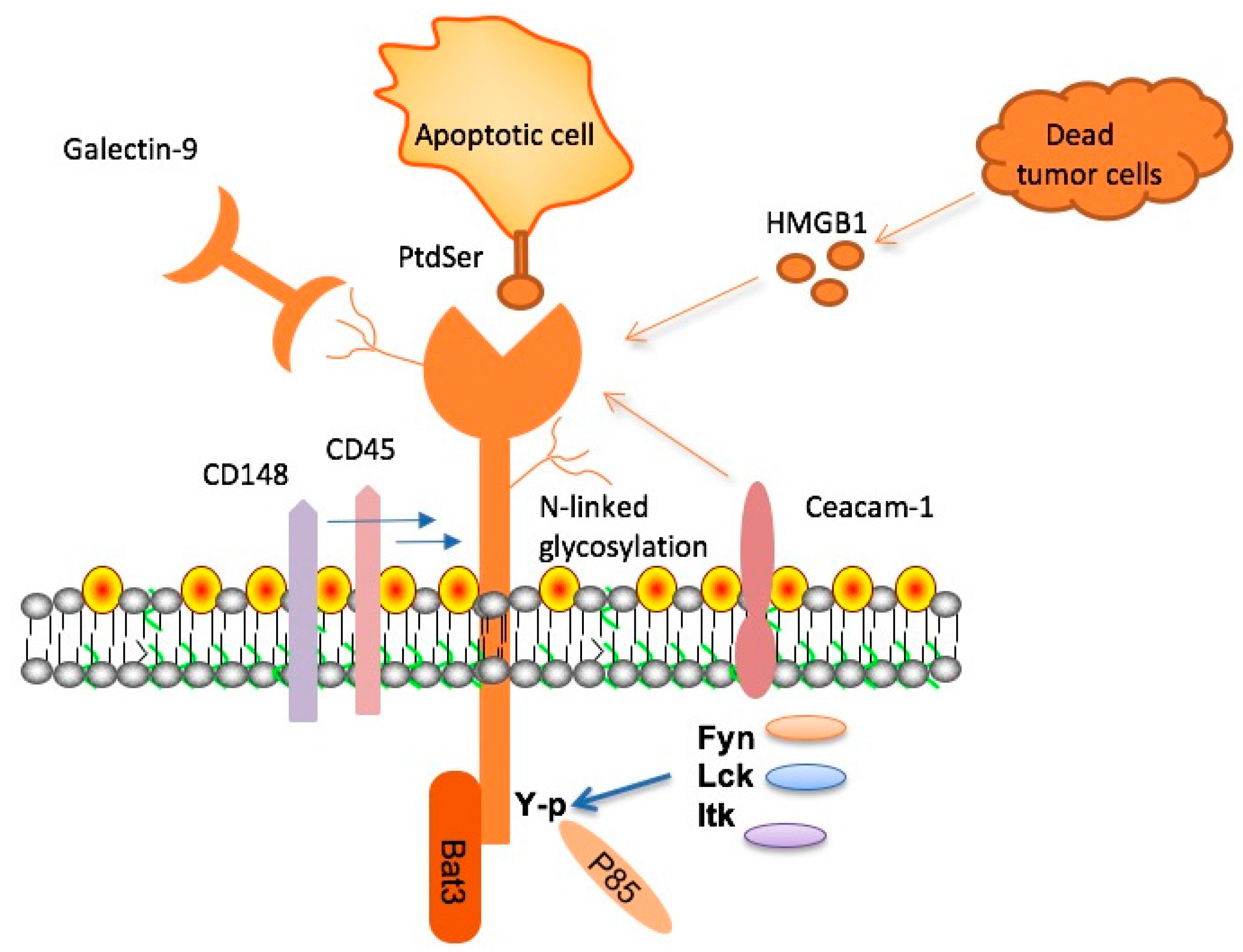
TIM-3 therapy represents a groundbreaking approach to Alzheimer’s disease by leveraging our understanding of immune system dynamics, particularly in late-onset Alzheimer’s. TIM-3, or T-cell Immunoglobulin Mucin-3, acts as a checkpoint molecule that inhibits microglia, the brain’s immune cells, from effectively clearing amyloid plaques. Recent research indicates that deleting the TIM-3 molecule allows these microglial cells to regain their function, leading to improved clearance of disease-related plaques and cognitive enhancements in animal models. This is particularly significant considering that the majority of Alzheimer’s cases are late-onset, emphasizing the potential impact of TIM-3 targeted therapies in this context.
By repurposing TIM-3 inhibitors, originally developed for cancer treatments, researchers aim to convert the negative regulatory effects of TIM-3 on microglia into a therapeutic advantage. In trials involving genetically modified mice lacking the TIM-3 gene, significant reductions in plaque levels and subsequent cognitive improvements were observed. This breakthrough could pave the way for novel treatments that not only target the biological underpinnings of Alzheimer’s disease but also enhance memory function, marking a promising shift in the quest for effective Alzheimer’s disease treatment.
Frequently Asked Questions
What is TIM-3 and how does it relate to Alzheimer’s disease treatment?
TIM-3 is a checkpoint molecule that regulates the immune response. In the context of Alzheimer’s disease, it inhibits microglia, the brain’s immune cells, from clearing toxic plaques. By targeting TIM-3, researchers aim to enhance cognitive improvement in Alzheimer’s patients by enabling microglia to attack and remove these plaques.
How does TIM-3 therapy improve cognitive function in Alzheimer’s disease?
TIM-3 therapy works by blocking the TIM-3 pathway, thus freeing microglia to effectively clear amyloid beta plaques from the brain. This process has shown promise in improving cognitive function during tests with lab mice, suggesting potential benefits for Alzheimer’s disease treatment.
What role do microglia play in Alzheimer’s and how does TIM-3 affect them?
Microglia serve as the brain’s immune defense, responsible for removing waste and plaques. TIM-3 inhibits their action, preventing them from effectively clearing amyloid plaques that contribute to Alzheimer’s disease. By targeting TIM-3, therapies aim to restore the microglia’s ability to prune these harmful plaques.
Can TIM-3 therapy be repurposed from cancer treatment for Alzheimer’s disease?
Yes, TIM-3 therapy can be repurposed from cancer treatment. Existing anti-TIM-3 antibodies that have been effective in cancer therapies are now being explored for their potential to clear amyloid plaques in Alzheimer’s disease, representing a promising new approach to treatment.
What evidence supports the efficacy of TIM-3 therapy in Alzheimer’s disease?
Preliminary studies conducted on genetically modified mice lacking the TIM-3 gene showed enhanced clearance of amyloid plaques and subsequent cognitive improvements. This indicates that targeting TIM-3 could provide a novel method for treating Alzheimer’s disease by improving the brain’s immune response.
What is the significance of the HAVCR2 gene in Alzheimer’s disease related to TIM-3?
The HAVCR2 gene encodes TIM-3 and has been identified as a genetic risk factor for late-onset Alzheimer’s disease. Variants of this gene lead to increased TIM-3 expression in microglia, which disrupts plaque clearance, making it a key target for therapeutic interventions.
What could a TIM-3 therapy for Alzheimer’s patients look like?
A TIM-3 therapy for Alzheimer’s patients may involve the use of anti-TIM-3 antibodies or small molecules designed to inhibit TIM-3’s inhibitory functions, thereby reactivating microglial cells to clear neurotoxic plaques more effectively.
How long has research into TIM-3 therapy for Alzheimer’s disease been in progress?
Research into TIM-3 therapy as a treatment for Alzheimer’s disease has been ongoing for about five years, involving multiple experiments and collaborations aimed at understanding its potential benefits in cognitive improvement and plaque clearance.
What are the next steps for TIM-3 therapy research in Alzheimer’s disease?
The next steps involve testing human anti-TIM-3 antibodies in mouse models engineered to replicate Alzheimer’s disease. This could provide insights into their effectiveness for halting plaque development and improving cognitive function in human patients.
| Key Point | Details |
|---|---|
| TIM-3 and Alzheimer’s Disease | TIM-3, an immune checkpoint molecule linked to Alzheimer’s, is expressed on microglia, inhibiting plaque clearance. |
| Research Findings | Deleting the TIM-3 gene in mice led to improved clearance of plaques and better cognitive performance. |
| Importance of Microglia | Microglia are brain immune cells that also prune synapses; increased TIM-3 inhibits plaque removal. |
| Potential Therapy | Using anti-TIM-3 antibodies could block the inhibitory effects of TIM-3 and enable effective plaque clearance in Alzheimer’s. |
| Future Directions | Studies are underway to see if human anti-TIM-3 can prevent plaque development in Alzheimer’s disease models. |
Summary
TIM-3 Therapy represents a promising avenue for Alzheimer’s disease treatment by targeting the TIM-3 molecule, which inhibits the brain’s microglia from clearing harmful plaques. Recent research demonstrates that when TIM-3 expression is reduced or eliminated, these microglial cells can effectively remove amyloid plaques, leading to improved cognitive function in animal models. As more studies are conducted to assess the viability of TIM-3 inhibitors in humans, there is renewed hope for patients suffering from Alzheimer’s, particularly in light of previous challenges faced by other therapeutic approaches.